
Healthcare Work Group/Healthy Weight Advisory Committee
Purpose
The purpose of the Healthcare Work Group/Healthy Weight Advisory Committee (hereinafter referred to as the Healthcare Work Group) is to increase support for and collaboration between healthcare professionals, healthcare systems and other stakeholders to promote the adoption of healthy lifestyle practices for improved health and prevention and treatment of obesity and obesity-related chronic diseases in Missourians across the lifespan. While previously two separate but related Work Groups, the Healthcare Work Group and the Healthy Weight Advisory Committee have decided to join into one group as they share common goals and members.
Overall Objective
Enhance healthcare professional training, collaboration and advocacy that improve health and prevent and treat obesity and obesity-related chronic diseases.
The obesity epidemic continues to increase in Missouri, which ranks 16th of 50 states with the highest rates of adult obesity in 2022. Missouri’s obesity rate in 2022 was 36.5% (an increase of nearly 25%) from 29.4% in 2011 (see figure 35 in Missouri State Health Assessment - MSHA).
Obesity in children and adults is increasingly being acknowledged as a complex and chronic medical condition with multiple biologic, social and environmental drivers requiring multi-disciplinary care. In addition, obesity is associated with several co-occurring conditions such as type 2 diabetes, hypertension, obstructive sleep apnea, liver dysfunction, and overall increased risk of cardiovascular disease. These conditions are seen across the lifespan. Optimal nutrition and physical activity are vital in both prevention and treatment strategies.
Health disparities can increase the risk of obesity among certain populations and they need to be taken into consideration, along with deeper understanding of the social drivers of health that can greatly affect the risk of obesity among individuals (figure 36, MSHA). This data, coupled with increasing time- and regulatory-related demands on healthcare professionals, suggest that additional resources and education are needed to assist Missouri healthcare professionals in addressing nutrition, physical activity and other related concerns among their patients. Mitigating the rise of both adult and pediatric obesity with evidence-based interventions that prevent and treat excess weight gain is critical.
Both healthcare professionals and patients face challenges concerning lifestyle change interventions. Healthcare professionals cite a lack of time to adequately address the topic during clinic visits, lack of resources, need to provide person-centered care, and a lack of knowledge about billable services for obesity treatment. Patients fear judgment about their own and their children’s obesity, experience damaging weight-related conversations and receive miseducation from social media and other sources.
Improving communication around the importance of physical activity and nutrition should be a priority for healthcare professionals across Missouri, as 2022 data suggests only 75% of Missouri adults get some level of physical activity outside of work (MSHA) and only 48% of Missouri high school students get 60+ minutes of physical activity daily (Youth Risk Behavior Survey 2021). Similarly, less than 35% of Missouri residents consume at least three servings of fruits and vegetables daily (MSHA).
Missouri Obesity Statewide Rate — 36.5%
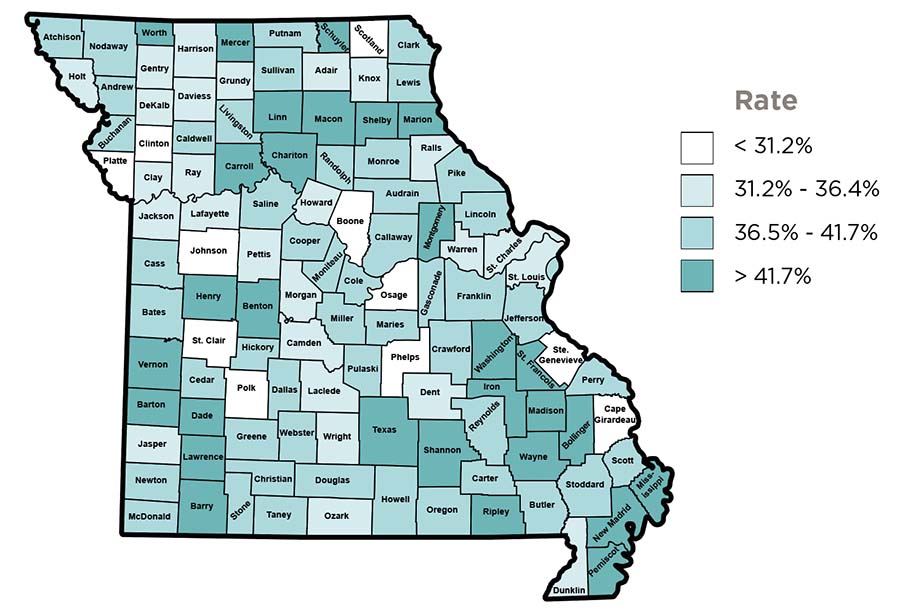
Source: Missouri Department of Health and Senior Services, Missouri County Level Study, 2022.
Collaboration is also needed amongst specialists in primary care, metabolic and bariatric care, physical activity, nutrition, mental health and public health professionals to develop and improve comprehensive, coordinated care.
With this knowledge, the healthcare Work Group aims to collaborate with several other Work Groups to enhance knowledge across these fields, and to promote dissemination of knowledge and resources to increase Missouri’s healthcare professional workforce capacity. The Work Group will pursue collaboration with federally funded initiatives, such as the State Physical Activity and Nutrition Program (SPAN) and the High Obesity Program (HOP). Further, the Work Group will seek to advocate across a wide range of key stakeholders to improve coverage of evidence-based obesity treatment and prevention services.
Goal
Increase awareness of the MOCAN Healthcare Work Group and enhance connections between the Work Group and existing and new agencies and organizations throughout Missouri to increase awareness, evaluation and treatment of obesity and obesity-related chronic diseases.
Objectives
- Maintain regular Work Group representation from key stakeholder organizations and expand representation from new key stakeholder organizations.
- Connect healthcare professionals across all age ranges and specialties, by maintaining and growing statewide health-related organization collaborations.
Evaluation Measures
- Healthcare Work Group attendance records, number of new organizations joining the healthcare Work Group, number of communications in internal and external newsletters and publications, number of speaking engagements in which information about MOCAN and the Work Group are included
- Number of communication features, number of collaborations, number of speaking engagements including discussion of collaborations
Timeline
- 2025 — Collect baseline data regarding MOCAN’s representation in various statewide agencies and organizations. Explore various healthcare professional collaboration options.
- 2026 — Increase our representation by 50% via informational blurbs in statewide organization newsletters and/or speaking engagements at statewide conferences.
- 2027-2030 — Continue to increase representation by 5% each year.
Goal
Develop, improve and deliver education to increase knowledge about evidence-based healthy lifestyles, obesity management and prevention and related social drivers of health.
Objectives
- Develop and/or identify discipline-specific resources about the multiple factors that contribute to healthy weight and the development and maintenance of obesity.
- Develop an obesity treatment and prevention toolkit for primary care providers to support their efficacy and confidence in addressing obesity with their patients. See appendix 1 for toolkit topics.
- Toolkit will be housed on the MOCAN Healthcare Work Group website and/or the MU Continuing Education for Health Professionals website and linked to other organizations.
- Connect with healthcare professional organizations and other organizations with connection to these professionals to promote relevant trainings and distribute obesity/healthy weight resources.
- This will include promoting the MTN PWM ECHO, including obesity as a topic in other related ECHOs and participation in local and state professional conferences and organizational meetings.
Evaluation Measures
- Number of resources, surveys, trainings and other educational opportunities developed or identified, number of training participants attending trainings, number of communication metrics promoting trainings and resources (email opens, clicks, etc.), number of champions cultivated as evidenced by tracking through the University of Missouri ECHO programs
- Number of resources distributed to healthcare professionals, number of types of healthcare professionals receiving resources and/or attending trainings
Timeline
- 2025 — Study/collect data on available opportunities for further education and what percentage are currently utilized. Set baseline for use of resources vs. utilization at 6/12/18/24 months.
- 2026 — Increase the number of healthcare professionals reached by 10%, complete toolkit production.
- 2027 — Increase the number of healthcare professionals reached by 20%; track downloads/clicks on toolkit using Qualtrics survey.
- 2028-2030 — Identify champions in each part of the state as resources to continue the work of educating in their communities. Increase toolkit utilization.
Goal
Increase access to treatment for obesity (FBT – family based behavioral treatment, IBT – intensive behavioral therapy, MNT – medical nutrition therapy).
Objectives
- Increase awareness of the existing MO HealthNet benefit for the treatment of obesity to healthcare professionals.
- Increase the workforce capacity for delivery of the MO HealthNet benefit.
- Support and educate behavioral health providers and registered dietitians on the existence of the benefit and methods of certification to be able to offer the MHN benefit and similar programs for patients. We will also support their referral process.
- Help to create a trained provider registry and collaborate with MHN on their credentialed provider database for referral networking and educate medical providers on the existence of the benefit and the steps to refer patients.
- Connect with MHN and MHN managed care organizations (MCOs) to improve knowledge of benefit among their members, streamline/make uniform information and resources.
- Work with MHN/MCOs to promote benefit to providers and provide information as well as working with MHN/MCOs to ease or waive the prior authorization process to make it less cumbersome for providers/clinics.
- Advocate to allow coverage for partial participation for those that cannot commit to the full participation requirements.
- Identify and promote best strategies to improve patient and family understanding of value of weight management and benefit available.
- Identify or develop communication strategies to facilitate discussion of obesity with patients and colleagues.
- Create pamphlets and other resources for healthcare professionals such as tips on how to talk about obesity and how to refer for MHN benefit.
- Create resources for patients/families such as the benefits of treating obesity, available treatment options.
Evaluation Measures
- Number of outreaches, such as number of promotional items sent, number of times benefit is mentioned in presentations
- Metrics such as: number of trainings developed and delivered; creation of trainee registry; number of trainings about benefit; Number of registered dietitian nutritionists and behavioral health specialists credentialed to offer the benefit; Number of MHN/MCO claims utilizing the benefit in collaboration with the MU Center for Health Policy and other agencies
- Number of communications, meetings and presentations, number of policy changes
- Number of resources created
Timeline
- 2025 — Continue working with MOHealthNet (MHN) to further delineate the certifications, trainings, and level of treatment experience acceptable for ability to treat. Review and advocate for models for telehealth/virtual visits for those areas where resources are very limited, or an ECHO model where dietitians/behavioral health specialists are available as resources to a local dietitian/behavioral health specialist, group visits virtually but may need to develop contracts between medical group/system and individual providers to offer more widespread visit capacity virtually. Connect with MHN and MCOs to alert them to current concerns with coverage for obesity treatment.
- 2026-2027 — Explore the potential for programs that may be available for community partnership such as online offerings. Assist healthcare professionals and systems to be able to contract with outside registered dietitian nutritionists and behavioral health providers, including a possible peer learning network available for FQHCs through MPCA. Further delineate credential requirements, with provider database functioning easily by the end of year 3. Advocate to MHN/MCOs to allow data about obesity diagnosis, evaluation and treatment to not rely solely on claims diagnosis codes but instead allow mechanisms for clinical data from the EHR to flow into their data systems (by the end of year 3).
- 2028-2030 — Monitor referral processes and if needed host listening sessions with providers and patients to troubleshoot concerns with referrals and the delivery of the benefit.
Goal
Advocate for comprehensive, multidisciplinary coverage of obesity prevention and treatment, intensive behavioral treatment, pharmacotherapy and weight loss surgery, and chronic disease management resources like scales, blood pressure cuffs, access to healthy nutrition and physical activity resources.
Objectives
- Identify and convene key stakeholders (e.g., insurers, patients, healthcare providers and systems, universities, legislators).
- Develop, support and monitor obesity advocacy strategies as well as establish evaluation mechanisms for tracking strategy efforts.
- Collaborate with existing resources and develop new collaborations to evaluate obesity treatment benefit reach, uptake, issues.
- Develop tools for healthcare professionals to support advocacy for improved access to care such as letters of medical necessity for coverage of anti-obesity medications, and how to navigate prior auth and insurance denials. Identify or develop coding and billing guidance, including resources from national healthcare professional organizations.
Evaluation Measures
- Number of stakeholders identified and approached along with meetings convened, especially with insurers
- Number of advocacy materials developed and percent increased coverage of obesity and other chronic disease management materials (as evidenced through MHN and PCHH, Medicaid managed care claims), data obtained through PWM ECHO program
- MHN and PCHH programs and data sources, Medicaid managed care organizations, DHSS, MHA, MPCA data, PWM ECHO data
- Number of resources developed and distributed to healthcare professionals. Number of resources accessed from MOCAN’s toolkit website, PWM ECHO data
Timeline
- 2025 — Complete identifying key stakeholders
- 2025-2027 — Convene to discuss obesity advocacy strategies and tracking systems
- 2028-2030 — Monitor the implementation and efficacy of tracking systems using data from PWM ECHO
Goal
Recognize individuals who are innovative in promoting nutrition and physical activity in their communities.
Objectives
- Offer annual healthcare award to pre-professional students or professionals increasing opportunities for physical activity and nutrition in their communities.
- Share nominations with MO DHSS State Health Improvement Plan staff and other statewide organizations, and solicit information from these stakeholders about HCP involvement.
- Offer opportunities for idea-sharing among Missouri agencies for improving healthcare professional-led efforts to improve physical activity and nutrition in their communities, including presentation times added to regular meetings to feature projects from different regions of the state and features in the MOCAN newsletter.
Evaluation Measures
- Number of channels through which award program is promoted, number of nominations received
- Number of nominations received and shared
- Number of members sharing projects/ideas in MOCAN and state organization newsletters, during Work Group and HWAC/Healthcare Work Group meetings and in other venues
Timeline
- 2025-2030 — Healthcare awards provided annually; increase opportunities for idea sharing among Missouri agencies by 10% each year