COLUMBIA, Mo. – Missouri ranks below the national average in many key measures related to health and access to health care, especially in rural parts of the state.
A new report from University of Missouri Extension suggests that “health entrepreneurship” might be one solution to the state’s shortage of care providers.
“Turnover is lower among primary health care providers when they practice as self-employed physicians instead of working as wage or salary employees,” said Sarah Low, associate professor of regional economics in MU’s Division of Applied Social Sciences.
The report, “Missouri Health Care Availability and Outcomes Differ Regionally,” was written by Low and Maria Kuhns, an MU Extension business development counselor and former MU graduate research assistant in agricultural and applied economics.
In her master’s thesis, Kuhns looked at survey data from more than 900 rural health care providers to find that, all things being equal, self-employed health care providers— “provider-entrepreneurs”—were 12% less likely to consider leaving their rural communities.
“Many young Missourians I talk to want to move back to their home communities,” Low said. But health care practitioners are often drawn away from rural communities to urban areas and other industries by more competitive pay.
Kuhns and Low say that expenses such as malpractice insurance discourage physicians from establishing private practices. They suggest that encouraging health entrepreneurship could expand the supply of nonphysician primary care providers such as nurse practitioners and physician assistants.
Allowing nurse practitioners in Missouri to set up independent practices, as recommended by the National Academy of Medicine, could create more opportunities for health entrepreneurship, Low said. Missouri is one of the 11 states that still restrict nurse practitioners from practicing independently.
Low said it might be easier for rural communities to attract and retain nurse practitioners compared to physicians. “One reason is economics,” she said. “Physicians carry high student loan debts. That gives them incentive to seek higher salaries, which rural communities can’t offer. Without this huge debt, nurse practitioners may be more likely to move back to their home communities and practice.”
Better access to health care is linked to factors such as higher life expectancy and lower prevalence of chronic conditions such as heart disease, diabetes, cancer and depression. More local access to health services can also benefit a community economically through a healthier workforce, creating jobs in the health care sector and making the community more attractive to potential employers and residents, Low said.
“Missouri Health Care Availability and Outcomes Differ Regionally” is available for free download at extension.missouri.edu/publications/mx56.
Extension and Engagement Week 2021 focuses on health
The four UM System universities, MU Extension, MU Health and statewide partners, stakeholders, agency leaders and legislators will gather virtually for Extension and Engagement Week, Oct. 18-23, 2021, to learn, brainstorm and create a plan for improving the health and well-being of the people of Missouri. Online events will explore health equity, the opioid crisis, rural health and data-informed health strategies with leaders and thinkers from around the state. Learn more at community.umsystem.edu.
Image available:
extension.missouri.edu/media/wysiwyg/Extensiondata/Pub/images/mx0056_fig02.png
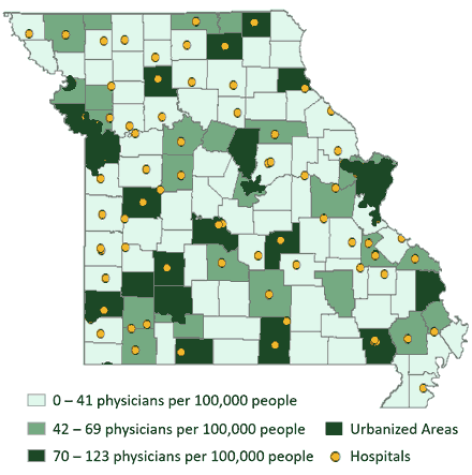
Rural Missouri Hospital Locations as of April 5, 2021. (Source: MU Extension Exceed map using U.S. DHS Homeland Infrastructure Foundation-Level data.)